Point of Care Ultrasound for Hernias
Originally Published: 2012-Feb-21
**This post was originally part of the ACEP Emergency Ultrasound Section’s Newletter in the Tips and Tricks section . The newsletter is located on the member only section of the site so I am posting here to make it more available.**
Patients commonly present with complaints of abdominal hernias and are frequent incidental findings in the emergency department. Incarcerated hernias can cause swelling, pain, and may require emergent surgical consultation if strangulated.
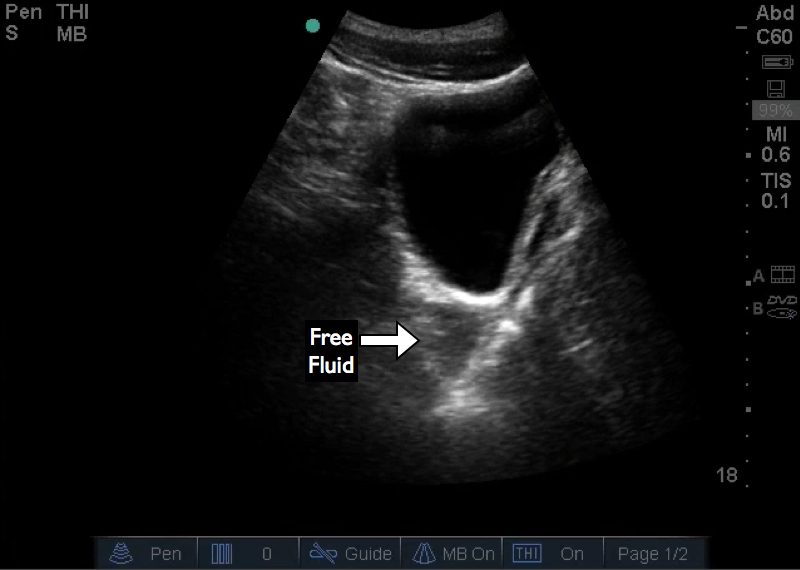
While an incarcerated hernia can be found on physical exam, ultrasound can assist in the management of these cases. Imaging the incarcerated hernia to identify the contents of hernia sac can help differentiate bowel from adipose tissue. As well, one can identify concomitant pathology such as free fluid, bowel wall thickening, pneumotosis coli, aperistalsis, and abnormal blood flow.
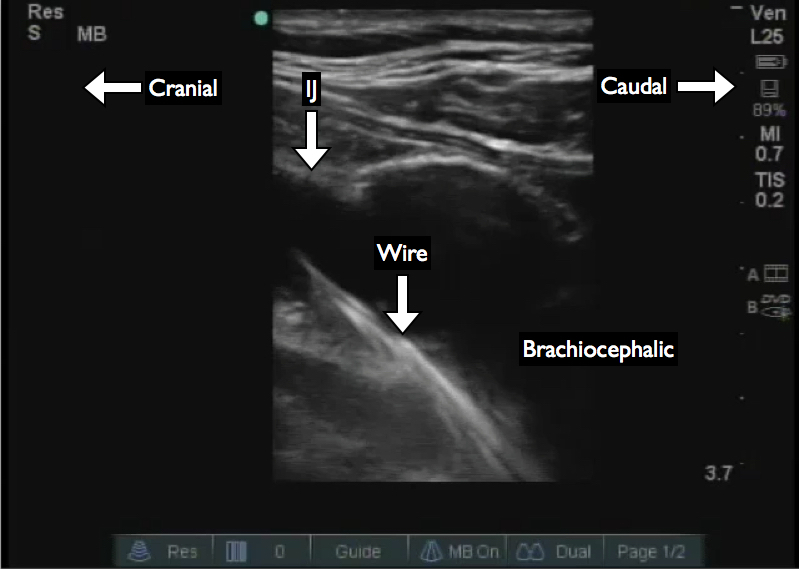
Diagnostic imaging is commonly described in many texts and articles; however, an additional step in the imaging protocol can help with the management of incarcerated hernias. Scan through the hernia sac and pay special attention to the abdominal wall for the break in the wall or the neck of hernia sac, this will allow planning for reduction. Identification of the neck allows the operator to direct the hernia contents toward the neck during manual reduction. It also allows the clinician to identify the size of the neck compared to the hernia contents.
Figure 1 shows an incarcerated ventral hernia containing small bowel. The neck can be identified by the defect in the abdominal wall. This hernia was successfully reduced by applying pressure from the lateral edge of the bowel loop toward the neck. Figure 2 shows the hernia post reduction containing only fat; the fascial defect is still visible.
While this large hernia had a midline neck, that is not always the case as demonstrated in Figure 3. The neck is visible and the hernia sac is laterally located. Evaluation of the hernia contents and neck location can aid in planning the reduction. Practice visualizing known hernias and the fascial defect or neck on patients with hernias that are not incarcerated or strangulated.
Figure 1: Incarcerated hernia with bowel and neck visualized
Figure 2: Post reductions fat containing hernia and neck are visualized
Figure 3: Small hernia lateral to the neck