Tips and Tricks for the Pelvic Views during the FAST Exam
Originally published: 2011-Apr-18
This is a short article that my colleagues and I wrote for the American College of Emergency Medicine Emergency Medicine Ultrasound Section April Newsletter.
The full newsletter can be found here.
The Focused Assessment with Sonography in Trauma or FAST exam is one of the most common Point of Care Ultrasound exams performed in the Emergency Department. As discussed in numerous forums, the FAST (or E-FAST) exam can be used in multiple clinical scenarios beyond the traumatically injured patient. We will discuss two common errors that can lead to the misdiagnosis of subtle findings.
The pelvic windows in the FAST exam are often scanned hastily if the RUQ and LUQ do not show free fluid; however, subtle pathology can be missed if the windows are not surveyed in a thorough manner.
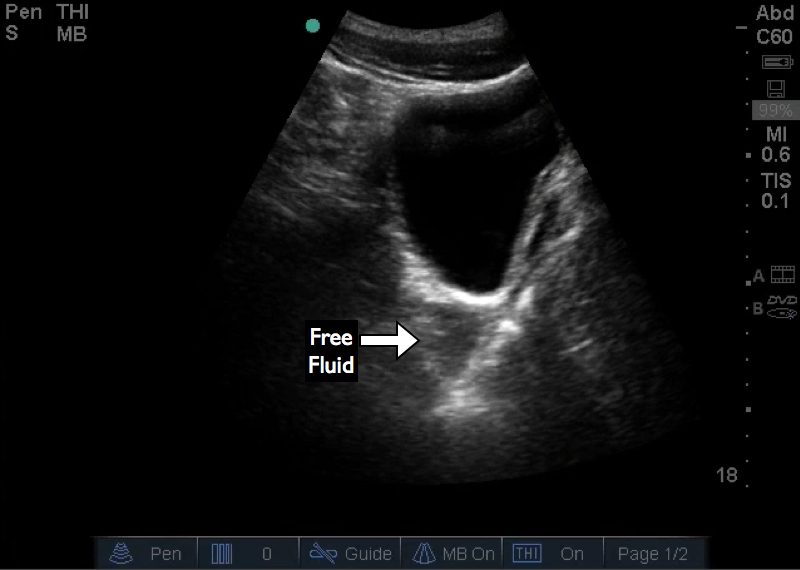
The urine-filled bladder results in posterior acoustic enhancement, which can obscure pelvic structures and pathology posterior to the bladder. This will be amplified if the far field gain is not appropriately adjusted. Structures may appear significantly more hyperechoic, and free fluid can be missed due to wash-out from an overgained far field image. Figure 1 is an example of missed pelvic free fluid due to posterior acoustic enhancement. The overgained far field obscures the free fluid.
Sagittal view of the bladder with free fluid. The posterior acoustic enhancement leads to an overgained far field despite the appropriate gain settings of the near field. This small amount of free fluid, caused by a liver injury, was missed on initial evaluation.
Figure 2 demonstrates a similar transverse view of the bladder, but with improved far field gain. Internal echoes are visible within the free fluid due to posterior acoustic enhancement; however, further reduction in far field gain may reduce visualization of anatomic structures. Sonographers must strike a balance between adjusting the far field gain to adequately visualize free fluid while still identifying posterior structures and boundaries. This highlights the need to remain vigilant in looking for small amounts of free fluid or other subtle findings. Despite the reduced far field gain and improved image, the persistent artifact within the fluid could mask this pathology. Appropriate imaging and assessment in the suprapubic window requires an understanding of both the pitfalls of posterior acoustic enhancement, as well as any limitations that can be encountered when correcting for this artifact.
Sagittal view of the bladder with subtle free fluid. Although the far field gain is better than Figure 1, there are still echoes within the free fluid due to posterior acoustic enhancement. This highlights the need to be vigilant for subtle findings in the FAST exam.
The second common error occurs while imaging the bladder in the transverse plane. Sonographers commonly fail to adequately visualize the lateral edges of the structure. One of the goals of transverse imaging is to evaluate for free fluid that is lateral to the bladder and may not be apparent on sagittal imaging. Figure 3 demonstrates this potential pitfall.
Transverse view of the bladder with free fluid located laterally to the bladder.
Figure 4 shows a transverse view in which the lateral edges are not visualized. This occurs most commonly either when the bladder is distended or when a small footprint transducer, such as the phased array or small curved array, is used. If this occurs, the lateral edges need to be evaluated by scanning each half of the bladder separately on transverse imaging.
Transverse image of the bladder using a phased array transducer. Due to the small footprint, the lateral edges of the bladder are not visualized and free fluid may not be visualized.