Single Operator Sterile Sheathing of an Ultrasound Probe for an Ultrasound Guided Procedure
Originally published 2011-Mar-07
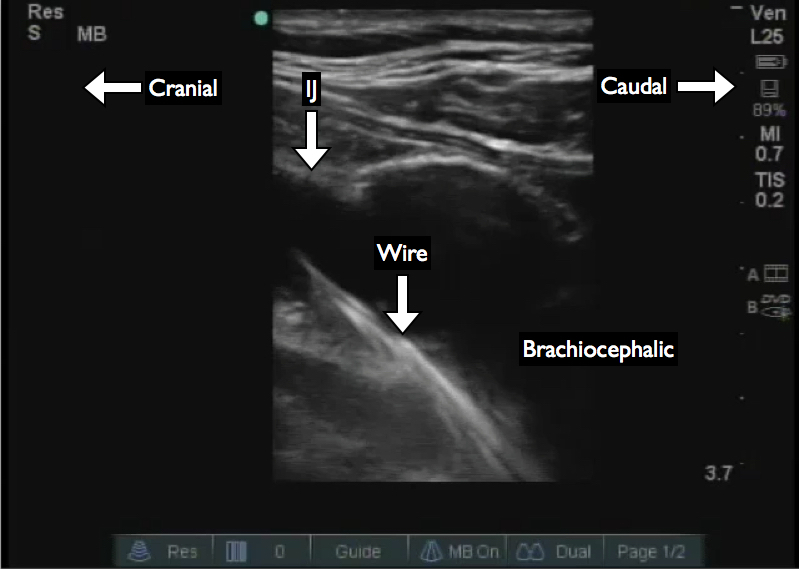
During the care of critically ill patients either in the Emergency Department or other settings can involve the placement of Central Venous Catheters. The literature supports the use of Ultrasound Guidance to prevent mechanical complications and increase success rates. However, in addition to mechanical complications the patients can be at risk for delayed complications such as central line associated blood stream infections, CLABSI, or line infections.
One method to reduce this is the use of full barrier sterile precautions. This includes placing the ultrasound probe in a sterile sheath to allow real-time guidance and maintaining the sterile field. Many sterile sheaths are not designed for a single operator placement in the way they are folded and packaged. This has lead to frustration, loss of sterility, infamous gel accident stories, and a reliance on an assistant. However, there is a method to sheath the probe and maintain the sterile field as a single operator.
The procedure can be broken down into the following steps:
- Place the probe upright in the holder
- Place adequate nonsterile gel on the probe surface
- Engage full barrier sterile precautions for the operator
- Open the sterile sheath and place on non-dominant hand
- Invert the sheath onto the dominant hand
- Grasp the top of the probe
- Unfurl the sheath onto the probe and cord
- Secure the sheath in place and smooth out air bubbles
- Place sterile gel on the sheath to allow imaging and procedural guidance
This was also published Academic Emergency Medicine in the Dynamic Emergency Medicine Section with an accompanying manuscript. Trotter M, Nomura JT, Sierzenski PR. Acad Emer 2010;17:e153.