Originally Published 2011-Jan-20
This is a short blurb that my colleagues and I wrote for the ACEP US Section Newsletter, January 2011 edition.
American College of Emergency Physicians Emergency Ultrasound Section Newsletter
Tips and Tricks Section January 2011
Christiana Care Health System Emergency Medicine Ultrasound Fellowship Program
DT Cook MD, JT Mink MD, JT Powell MD, PR Sierzenski MD RDMS, and JT Nomura MD RDMS
Placement of a central line is a common procedure in the resuscitation of critically ill patients in the Emergency Department. Real-time ultrasound guidance can reduce mechanical complications associated with central venous cannulation. This includes decreasing arterial puncture and increasing the rate of first pass success.
One complication of central venous catheter placement that may be detected by ultrasound guidance of vessel cannulation is misdirection of the catheter. We have all had internal jugular (IJ) catheters that travel into the subclavian or flip in a retrograde direction. We can employ ultrasound to gauge direction of the needle, location of the bevel and direction of the guidewire J-Tip.
When cannulating the IJ you can evaluate the placement of the guidewire to ensure it is placed correctly. The first step is to make certain that the wire has been placed in the IJ without puncture of the posterior wall. As described in several publications visualization of the wire should occur in a transverse and sagittal plane to ensure its location of prior to dilation.
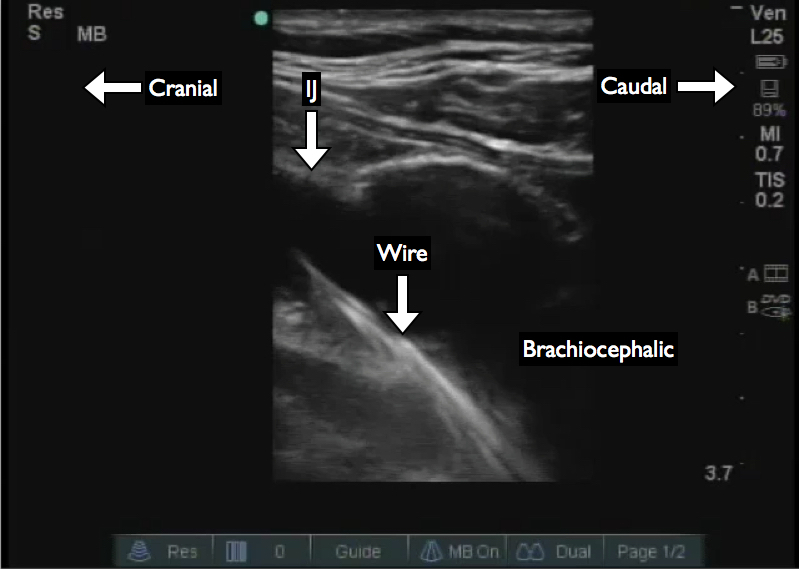
You can then angle the transducer and trace the IJ and wire to the brachiocephalic vein (Figure 1). Depending on the maximal depth and frequency of your probe you may or may not be able to visualize the superior vena cava. The next step is to evaluate the ipsilateral subclavian vein to ensure the wire is not directed laterally (Figure 2). You have now ensured that the wire is at least directed to the ipsilateral brachiocephalic.
If you prep widely enough you can also repeat this on the contralateral side to ensure that you have not directed the wire to the contralateral subclavian or IJ.